by Prakash Tyagi*
Clearly, TB continues to be a major global public health challenge, particularly in low and middle-income countries. Caused by mycobacterium tuberculosis, it can affect any part of the body, such as the brain, kidney or spine, but its most usual location within the human body is the lungs, this is because the infection is airborne and spreads mainly through the respiratory tract. TB can exist in a latent form known as latent TB infection (LTBI) or as TB disease with distinct clinical manifestations. If not diagnosed early and fully cured, TB infection can be fatal.
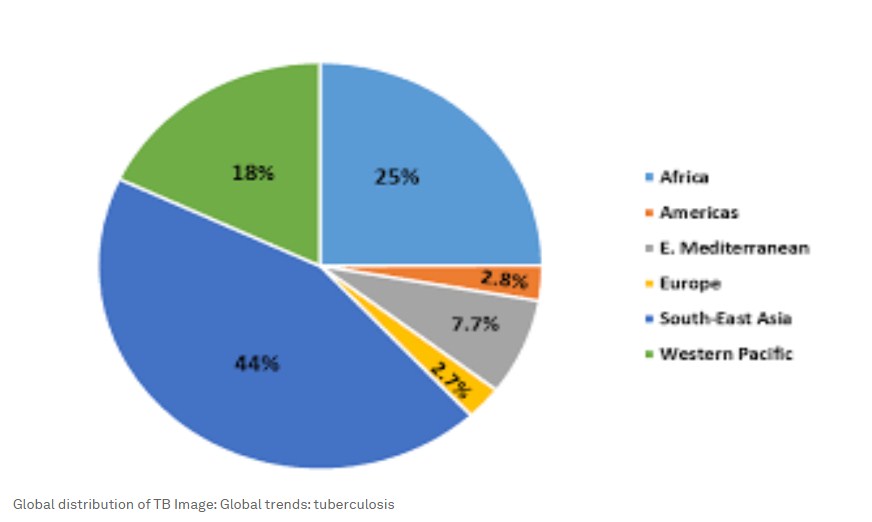
According to a WHO estimate, nearly 10.6 million people fell ill with TB in 2021 worldwide, out of which there were about six million men, about 3.4 million women and about 1.2 million children. Over 1.6 million people died from TB in 2021, making it the 13th leading cause of death worldwide and the second leading cause of death by an infectious disease after COVID-19.
The correlation between poverty and TB infection
Poverty is an important factor behind the spread of TB. Crowded and poorly ventilated living conditions and under-nutrition causing reduced resistance against infections are two critical contributors to TB spread. Low health awareness levels and a lack of primary healthcare services add to the challenge. In addition, co-morbidities such as HIV and silicosis in vulnerable populations, causing severe complexities, have also been a matter of concern in the battle against TB.
Over 80% of TB cases and deaths are registered in low- and middle-income countries. As such, migrant workers, labourers including mineworkers, prisoners, people with mental health challenges and older people, are particularly at risk. Poverty alleviation programmes and community development interventions play an important role in reducing TB, as these address the vulnerabilities significantly.
Drug-resistant TB strains pose further challenges
Multiple Drug Resistant TB, or MDR TB, is another major challenge that adversely impacts overall TB control efforts. MDR TB is a condition that does not respond to at least two drugs – isoniazid and rifampicin, the two most powerful antibiotics against TB. Even more difficult is Extensively Drug Resistant TB or XDR TB. MDR TB and XDR TB often are a result of mismanaged TB treatment and are difficult to manage with limited treatment options. China, India and Russia have the highest burden of MDR TB and XDR TB.
In India and in many other parts of the world, there is a large mineworkers’ population working in unsafe conditions amid health risks, who are prone to silicosis, a dust-born disease affecting the lungs. Mineworkers are highly susceptible to developing silicosis, which is incurable and leads to premature death. Silicosis patients are at a higher risk of developing pulmonary TB and often are affected by both silicosis and TB, known as silico-tuberculosis.
Evidently, TB is a disease that has a deep impact on vulnerable populations. Its magnitude with a large number of people affected by the disease is a massive public health concern. COVID-19 and its dramatic spread around the world caused further damage to TB control efforts worldwide and to the recent progress made on TB control. Understandably, there have been notable delays in the supply and delivery of TB control drugs, reduced intensity and coverage of TB education programmes and an inadequate focus on TB by health workers in the community burdened by pandemic-related priorities. As a result, there were significant declines in key TB programmatic results between 2019 and 2020. The number of people treated for drug-resistant TB fell by 19% and for extensively drug-resistant TB by 37%. It is feared that more harm may be caused to progress made on TB control as health systems and communities continue dealing with COVID-19 for years to come.
Creating an integrated approach to TB prevention and management
A more integrated approach to TB prevention and management that focuses on scaling up adaptation and mitigation efforts is needed. Several Civil Society Organizations (CSOs) are leading TB control efforts at the community level. GRAVIS, in India, has been addressing the challenges related to TB and silicosis in remote areas among the most vulnerable groups. The components of its approach include:
1. The formation and strengthening of Community-Based Organizations (CBO) – such as Self Help Groups (SHGs), Inter-Generational Learning Groups (ILGs) and Village Health Committees (VHCs) – who then act as TB educators within their communities.
2. The organization of TB sensitisation events and activities with a greater focus on MDR TB, XDR TB and silicosis.
3. Facilitating diagnostic and medical support to TB patients through GRAVIS medical services and through referral linkages with the Directly Observed Treatment Short-Course (DOTS) programme of the Government of India. GRAVIS has documented its work on lung health through various studies. Its programme on TB prevention and management reaches over 1.5 million people in rural India.
Looking ahead, the gaps that cause delays and inadequacies in TB control efforts will have to be looked into and must be bridged. TB control efforts need more hands, human resources and partners and hence more CSOs and CBOs need to join the efforts. They will need to be provided with orientation, hand-holding support and knowledge upgrades to be effective within their communities. Secondly, community-based cadres of health workers and TB champions must be strengthened further to enable them to lead educational and referral activities more effectively, reaching the last mile and the unreached. Thirdly, a holistic approach must be adopted with a strong focus on key contributing factors, such as nutritional education and support and on highlighting co-morbidities, such as silicosis and HIV.
World TB Day on March 24, 2023, has the theme of Yes! We can end TB! This is an important occasion for renewing the commitment and energy towards The End TB Strategy.
*Founder-Director, GRAVIS Hospital; Executive Director, GRAVIS
**first published in: Weforum.org




 By: N. Peter Kramer
By: N. Peter Kramer
