by Francesca Colombo, Helen E. Clark, Helena Legido-Quigley, Maliha Hashmi, Jan Kimpen, Paul Murray, Andre Goy, Pascal Frohlicher, Ian Wijaya, John E. Ataguba, Matthew Guilford, Sarah Ziegler, Ninie Wang, Donald Berwick, Nicola Bedlington and David Duong
Introduction
Our healthy future cannot be achieved without putting the health and wellbeing of populations at the centre of public policy.
Ill health worsens an individual’s economic prospects throughout the lifecycle. For young infants and children, ill health affects their capacity to acumulate human capital; for adults, ill health lowers quality of life and labour market outcomes, and disadvantage compounds over the course of a lifetime.
And, yet, with all the robust evidence available that good health is beneficial to economies and societies, it is striking to see how health systems across the globe struggled to maximise the health of populations even before the COVID-19 pandemic – a crisis that has further exposed the stresses and weaknesses of our health systems. These must be addressed to make populations healthier and more resilient to future shocks.
Each one of us, at least once in our lives, is likely to have been frustrated with care that was inflexible, impersonal and bureaucratic. At the system level, these individual experiences add up to poor safety, poor care coordination and inefficiencies – costing millions of lives and enormous expense to societies.
This state of affairs contributes to slowing down the progress towards achieving the sustainable development goals to which all societies, regardless of their level of economic development, have committed.
Many of the conditions that can make change possible are in place. For example, ample evidence exists that investing in public health and primary prevention delivers significant health and economic dividends. Likewise, digital technology has made many services and products across different sectors safe, fast and seamless. There is no reason why, with the right policies, this should not happen in health systems as well. Think, for example, of the opportunities to bring high quality and specialised care to previously underserved populations. COVID-19 has accelerated the development and use of digital health technologies. There are opportunities to further nurture their use to improve public health and disease surveillance, clinical care, research and innovation.
To encourage reform towards health systems that are more resilient, better centred around what people need and sustainable over time, the Global Future Council on Health and Health Care has developed a series of stories illustrating why change must happen, and why this is eminently possible today. While the COVID-19 crisis is severally challenging health systems today, our healthy future is – with the right investments – within reach.
1. Five changes for sustainable health systems that put people first
The COVID-19 crisis has affected more than 188 countries and regions worldwide, causing large-scale loss of life and severe human suffering. The crisis poses a major threat to the global economy, with drops in activity, employment, and consumption worse than those seen during the 2008 financial crisis. COVID-19 has also exposed weaknesses in our health systems that must be addressed. How?
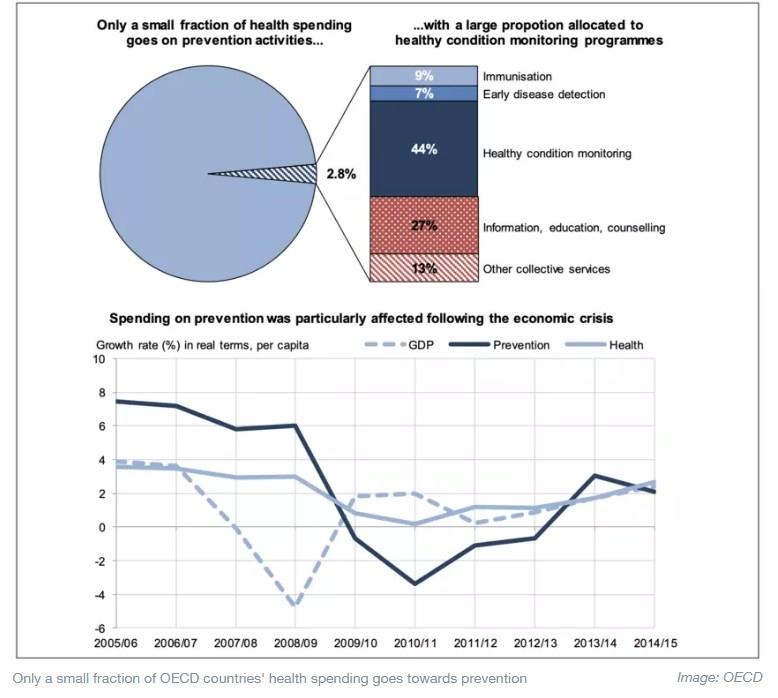
For a start, greater investment in population health would make people, particularly vulnerable population groups, more resilient to health risks. The health and socio-economic consequences of the virus are felt more acutely among disadvantaged populations, stretching a social fabric already challenged by high levels of inequalities. The crisis demonstrates the consequences of poor investment in addressing wider social determinants of health, including poverty, low education and unhealthy lifestyles. Despite much talk of the importance of health promotion, even across the richer OECD countries barely 3% of total health spending is devoted to prevention. Building resilience for populations also requires a greater focus on solidarity and redistribution in social protection systems to address underlying structural inequalities and poverty.
Beyond creating greater resilience in populations, health systems must be strengthened.
High-quality universal health coverage (UHC) is paramount. High levels of household out-of-pocket payments for health goods and services deter people from seeking early diagnosis and treatment at the very moment they need it most. Facing the COVID-19 crisis, many countries have strengthened access to health care, including coverage for diagnostic testing. Yet others do not have strong UHC arrangements. The pandemic reinforced the importance of commitments made in international fora, such as the 2019 High-Level Meeting on Universal Health Coverage, that well-functioning health systems require a deliberate focus on high-quality UHC. Such systems protect people from health threats, impoverishing health spending, and unexpected surges in demand for care.
Second, primary and elder care must be reinforced. COVID-19 presents a double threat for people with chronic conditions. Not only are they at greater risk of severe complications and death due to COVID-19; but also the crisis creates unintended health harm if they forgo usual care, whether because of disruption in services, fear of infections, or worries about burdening the health system. Strong primary health care maintains care continuity for these groups. With some 94% of deaths caused by COVID-19 among people aged over 60 in high-income countries, the elder care sector is also particularly vulnerable, calling for efforts to enhance control of infections, support and protect care workers and better coordinate medical and social care for frail elderly.
Third, the crisis demonstrates the importance of equipping health systems with both reserve capacity and agility. There is an historic underinvestment in the health workforce, with estimated global shortages of 18 million health professionals worldwide, mostly in low- and middle-income countries. Beyond sheer numbers, rigid health labour markets make it difficult to respond rapidly to demand and supply shocks. One way to address this is by creating a “reserve army” of health professionals that can be quickly mobilised. Some countries have allowed medical students in their last year of training to start working immediately, fast-tracked licenses and provided exceptional training. Others have mobilised pharmacists and care assistants. Storing a reserve capacity of supplies such as personal protection equipment, and maintaining care beds that can be quickly transformed into critical care beds, is similarly important.
Fourth, stronger health data systems are needed. The crisis has accelerated innovative digital solutions and uses of digital data, smartphone applications to monitor quarantine, robotic devices, and artificial intelligence to track the virus and predict where it may appear next. Access to telemedicine has been made easier. Yet more can be done to leverage standardised national electronic health records to extract routine data for real-time disease surveillance, clinical trials, and health system management. Barriers to full deployment of telemedicine, the lack of real-time data, of interoperable clinical record data, of data linkage capability and sharing within health and with other sectors remain to be addressed.
Fifth, an effective vaccine and successful vaccination of populations around the globe will provide the only real exit strategy. Success is not guaranteed and there are many policy issues yet to be resolved. International cooperation is vital. Multilateral commitments to pay for successful candidates would give manufacturers certainty so that they can scale production and have vaccine doses ready as quickly as possible following marketing authorisation, but could also help ensure that vaccines go first to where they are most effective in ending the pandemic. Whilst leaders face political pressure to put the health of their citizens first, it is more effective to allocate vaccines based on need. More support is needed for multilateral access mechanisms that contain licensing commitments and ensure that intellectual property is no barrier to access, commitments to technology transfer for local production, and allocation of scarce doses based on need.
The pandemic offers huge opportunities to learn lessons for health system preparedness and resilience. Greater focus on anticipating responses, solidarity within and across countries, agility in managing responses, and renewed efforts for collaborative actions will be a better normal for the future.
2. Improving population health and building healthy societies in times of COVID-19
The COVID-19 pandemic has been a stark reminder of the fragility of population health worldwide; at time of writing, more than 1 million people have died from the disease. The pandemic has already made evident that those suffering most from COVID-19 belong to disadvantaged populations and marginalised communities. Deep-rooted inequalities have contributed adversely to the health status of different populations within and between countries. Besides the direct and indirect health impacts of COVID-19 and the decimation of health systems, restrictions on population movement and lockdowns introduced to combat the pandemic are expected to have economic and social consequences on an unprecedented scale.
Population health – and addressing the consequences of COVID-19 – is about improving the physical and mental health outcomes and wellbeing of populations locally, regionally and nationally, while reducing health inequalities.? Moreover, there is an increasing recognition that societal and environmental factors, such as climate change and food insecurity, can also influence population health outcomes.
The experiences of Maria, David, and Ruben – as told by Spanish public broadcaster RTVE – exemplify the real challenges that people living in densely populated urban areas have faced when being exposed to COVID-19.?
Maria is a Mexican migrant who has just returned from Connecticut to the Bronx. Her partner Jorge died in Connecticut from COVID-19. She now has no income and is looking for an apartment for herself and her three children. When Jorge became ill, she took him to the hospital, but they would not admit him and he was sent away to be cared for by Maria at home with their children. When an ambulance eventually took him to hospital, it was too late. He died that same night, alone in hospital. She thinks he had diabetes, but he was never diagnosed. They only had enough income to pay the basic bills. Maria is depressed, she is alone, but she knows she must carry on for her children. Her 10-year old child says that if he could help her, he would work. After three months, she finds an apartment.
David works as a hairdresser and takes an overcrowded train every day from Leganes to Chamberi in the centre of Madrid. He lives in a small flat in San Nicasio, one of the poorest working-class areas of Madrid with one of the largest ageing populations in Spain. The apartments are very small, making it difficult to be in confinement, and all of David’s neighbours know somebody who has been a victim of COVID-19. His father was also a hairdresser. David’s father was not feeling well; he was taken to hospital by ambulance, and he died three days later. David was not able to say goodbye to his father. Unemployment has increased in that area; small local shops are losing their customers, and many more people are expecting to lose their jobs.
Ruben lives in Iztapalapa in Mexico City with three children, a daughter-in-law and five grandchildren. Their small apartment has few amenities, and no running water during the evening. At three o’clock every morning, he walks 45 minutes with his mobile stall to sell fruit juices near the hospital. His daily earnings keep the family. He goes to the central market to buy fruit, taking a packed dirty bus. He thinks the city’s central market was contaminated at the beginning of the pandemic, but it could not be closed as it is the main source of food in the country. He has no health insurance, and he knows that as a diabetic he is at risk, but medication for his condition is too expensive. He has no alternative but to go to work every day: "We die of hunger or we die of COVID."
These real stories highlight the issues that must be addressed to reduce persistent health inequalities and achieve health outcomes focusing on population health. The examples of Maria, David and Ruben show the terrible outcomes COVID-19 has had for people living in poverty and social deprivation, older people, and those with co-morbidities and/or pre-existing health conditions. All three live in densely populated urban areas with poor housing, and have to travel long distances in overcrowded transport. Maria’s loss of income has had consequences for her housing security and access to healthcare and health insurance, which will most likely lead to worse health conditions for her and her children. Furthermore, all three experienced high levels of stress, which is magnified in the cases of Maria and David who were unable to be present when their loved ones died.
The COVID-19 pandemic has made it evident that to improve the health of the population and build healthy societies, there is a need to shift the focus from illness to health and wellness in order to address the social, political and commercial determinants of health; to promote healthy behaviours and lifestyles; and to foster universal health coverage.² Citizens all over the world are demanding that health systems be strengthened and for governments to protect the most vulnerable. A better future could be possible with leadership that is able to carefully consider the long-term health, economic and social policies that are needed.
In order to design and implement population health-friendly policies, there are three prerequisites. First, there is a need to improve understanding of the factors that influence health inequalities and the interconnections between the economic, social and health impacts. Second, broader policies should be considered not only within the health sector, but also in other sectors such as education, employment, transport and infrastructure, agriculture, water and sanitation. Third, the proposed policies need to be designed through involving the community, addressing the health of vulnerable groups, and fostering inter-sectoral action and partnerships.
Finally, within the UN’s Agenda 2030, Sustainable Development Goal (SDG) 3 sets out a forward-looking strategy for health whose main goal is to attain healthier lives and wellbeing. The 17 interdependent SDGs offer an opportunity to contribute to healthier, fairer and more equitable societies from which both communities and the environment can benefit.
3. Imagine a ’well-care’ system that invests in keeping people healthy
Imagine a patient named Emily. Emily is aged 32 and I’m her doctor.
Emily was 65lb (29kg) above her ideal body weight, pre-diabetic and had high cholesterol. My initial visit with Emily was taken up with counselling on lifestyle changes, mainly diet and exercise; typical advice from one’s doctor in a time-pressured 15-minute visit. I had no other additional resources, incentives or systems to support me or Emily to help her turn her lifestyle around.
I saw Emily eight months later, not in my office, but in the hospital emergency room. Her husband accompanied her – she was vomiting, very weak and confused. She was admitted to the intensive care unit, connected to an insulin drip to lower her blood sugar, and diagnosed with type 2 diabetes. I talked to Emily then, emphasizing that the new medications for diabetes would only control the sugars, but she still had time to reverse things if she changed her lifestyle. She received further counselling from a nutritionist.
Over the years, Emily continued to gain weight, necessitating higher doses of her diabetes medication. More emergency room visits for high blood sugars ensued, she developed infections of her skin and feet, and ultimately, she developed kidney disease because of the uncontrolled diabetes. Ten years after I met Emily, she is 78lb (35kg) above her ideal body weight; she is blind and cannot feel her feet due to nerve damage from the high blood sugars; and she will soon need dialysis for her failing kidneys. Emily’s deteriorating health has carried a high financial cost both for herself and the healthcare system. We have prevented her from dying and extended her life with our interventions, but each interaction with the medical system has come at significant cost – and those costs will only rise. But we have also failed Emily by allowing her diabetes to progress. We know how to prevent this, but neither the right investments nor incentives are in place.
Emily could have been a real patient of mine. Her sad story will be familiar to all doctors caring for chronically ill patients. Unfortunately, patients like Emily are neglected by health systems across the world today. The burden of chronic disease is increasing at alarming rates. Across the OECD nearly 33% of those over 15 years live with one or more chronic condition, rising to 60% for over-65s. Approximately 50% of chronic disease deaths are attributed to cardiovascular disease (CVD). In the coming decades, obesity, will claim 92 million lives in the OECD while obesity-related diseases will cut life expectancy by three years by 2050.
These diseases can be largely prevented by primary prevention, an approach that emphasizes vaccinations, lifestyle behaviour modification and the regulation of unhealthy substances. Preventative interventions have been efficacious. For obesity, countries have effectively employed public awareness campaigns, health professionals training, and encouragement of dietary change (for example, limits on unhealthy foods, taxes and nutrition labelling).?,? Other interventions, such as workplace health-promotion programmes, while showing some promise, still need to demonstrate their efficacy.
The COVID-19 crisis provides the ultimate incentive to double down on the prevention of chronic disease. Most people dying from COVID-19 have one or more chronic disease, including obesity, CVD, diabetes or respiratory problems – diseases that are preventable with a healthy lifestyle. COVID-19 has highlighted structural weaknesses in our health systems such as the neglect of prevention and primary care.
While the utility of primary prevention is understood and supported by a growing evidence base, its implementation has been thwarted by chronic underinvestment, indicating a lack of societal and governmental prioritization. On average, OECD countries only invest 2.8% of health spending on public health and prevention. The underlying drivers include decreased allocation to prevention research, lack of awareness in populations, the belief that long-run prevention may be more costly than treatment, and a lack of commitment by and incentives for healthcare professionals. Furthermore, public health is often viewed in a silo separate from the overall health system rather than a foundational component.
Health benefits aside, increasing investment in primary prevention presents a strong economic imperative. For example, obesity contributes to the treatment costs of many other diseases: 70% of diabetes costs, 23% for CVD and 9% for cancers. Economic losses further extend to absenteeism and decreased productivity.
Fee-for-service models that remunerate physicians based on the number of sick patients they see, regardless the quality and outcome, dominate healthcare systems worldwide. Primary prevention mandates a payment system that reimburses healthcare professionals and patients for preventive actions. Ministries of health and governmental leaders need to challenge skepticism around preventive interventions, realign incentives towards preventive actions and those that promote healthy choices by people. Primary prevention will eventually reduce the burden of chronic diseases on the healthcare system.
As I reflect back on Emily and her life, I wonder what our healthcare system could have done differently. What if our healthcare system was a well-care system instead of a sick-care system? Imagine a different scenario: Emily, a 32 year old pre-diabetic, had access to a nutritionist, an exercise coach or health coach and nurse who followed her closely at the time of her first visit with me. Imagine if Emily joined group exercise classes, learned where to find healthy foods and how to cook them, and had access to spaces in which to exercise and be active. Imagine Emily being better educated about her diabetes and empowered in her healthcare and staying healthy. In reality, it is much more complicated than this, but if our healthcare systems began to incentivize and invest in prevention and even rewarded Emily for weight loss and healthy behavioural changes, the outcome might have been different. Imagine Emily losing weight and continuing to be an active and contributing member of society. Imagine if we invested in keeping people healthy rather than waiting for people to get sick, and then treating them. Imagine a well-care system.
4. Why early detection and diagnosis is critical
Although healthcare systems around the world follow a common and simple principle and goal – that is, access to affordable high-quality healthcare – they vary significantly, and it is becoming increasingly costly to provide this access, due to ageing populations, the increasing burden of chronic diseases and the price of new innovations.
Governments are challenged by how best to provide care to their populations and make their systems sustainable. Neither universal health, single payer systems, hybrid systems, nor the variety of systems used throughout the US have yet provided a solution. However, systems that are ranked higher in numerous studies, such as a 2017 report by the Commonwealth Fund, typically include strong prevention care and early-detection programmes. This alone does not guarantee a good outcome as measured by either high or healthy life expectancy. But there should be no doubt that prevention and early detection can contribute to a more sustainable system by reducing the risk of serious diseases or disorders, and that investing in and operationalizing earlier detection and diagnosis of key conditions can lead to better patient outcomes and lower long-term costs.
To discuss early detection in a constructive manner it makes sense to describe its activities and scope. Early detection includes pre-symptomatic screening and treatment immediately or shortly after first symptoms are diagnosed. Programmes may include searching for a specific disease (for example, HIV/AIDS or breast cancer), or be more ubiquitous. Prevention, which is not the focus of this blog, can be interpreted as any activities undertaken to avoid diseases, such as information programmes, education, immunization or health monitoring.
Expenditures for prevention and early detection vary by country and typically range between 1-5% of total health expenditures.? During the 2008 global financial crisis, many countries reduced preventive spending. In the past few years, however, a number of countries have introduced reforms to strengthen and promote prevention and early detection. Possibly the most prominent example in recent years was the introduction of the Affordable Care Act in the US, which placed a special focus on providing a wide range of preventive and screening services. It lists 63 distinct services that must be covered without any copayment, co-insurance or having to pay a deductible.
Whilst logic dictates that investment in early detection should be encouraged, there are a few hurdles and challenges that need to be overcome and considered. We set out a few key criteria and requirements for an efficient early detection program:
1. Accessibility
The healthcare system needs to provide access to a balanced distribution of physicians, both geographically (such as accessibility in rural areas), and by specialty. Patients should be able to access the system promptly without excessive waiting times for diagnoses or elective treatments. This helps mitigate conditions or diseases that are already quite advanced or have been incubating for months or even years before a clinical diagnosis. Access to physicians varies significantly across the globe from below one to more than 60 physicians per 10,000 people.² One important innovation for mitigating access deficiencies is telehealth. This should give individuals easier access to health-related services, not only in cases of sickness but also to supplement primary care.
2. Early symptoms and initial diagnosis
Inaccurate or delayed initial diagnoses present a risk to the health of patients, can lead to inappropriate or unnecessary testing and treatment, and represents a significant share of total health expenditures. A medical second opinion service, especially for serious medical diagnoses, which can occur remotely, can help improve healthcare outcomes.
Moreover, studies show that early and correct diagnosis opens up a greater range of curative treatment options and can reduce costs (e.g. for colon cancer, stage-four treatment costs are a multiple of stage-one treatment costs).³
3. New technology
New early detection technologies can improve the ability to identify symptoms and diseases early:
i. Advances in medical monitoring devices and wearable health technology, such as ECG and blood pressure monitors and biosensors, enable patients to take control of their own health and physical condition. This is an important trend that is expected to positively contribute to early detection, for example in atrial fibrillation and Alzheimers’ disease.
ii. Diagnostic tools, using new biomarkers such as liquid biopsies or volatile organic compounds, together with the implementation of machine learning, can play an increasing role in areas such as oncology or infectious diseases.?
4. Regulation and Intervention
Government regulation and intervention will be necessary to set ranges of normality, to prohibit or discourage overdiagnosis and to reduce incentives for providers to overtreat patients or to follow patients’ inappropriate requests. In some countries, such as the US, there has been some success through capitation models and value-based care.
Governments might also need to intervene to de-risk the innovation paradigm, such that private providers of capital feel able to invest more in the development of new detection technologies, in addition to proven business models in novel therapeutics.
5. The business case for private investment in healthcare for all
Faith, a mother of two, has just lost another customer. Some households where she is employed to clean, in a small town in South Africa, have little understanding of her medical needs. As a type 2 diabetes patient, this Zimbabwean woman visits the public clinic regularly, sometimes on short notice. At her last visit, after spending hours in a queue, she was finally told that the doctor could not see her. To avoid losing another day of work, she went to the local general practitioner to get her script, paying more than three daily wages for consultation and medication. Sadly, this fictional person reflects a reality for many people in middle-income countries.
Achieving universal health coverage by 2030, a key UN Sustainable Development Goal (SDG), is at risk. The World Bank has identified a $176 billion funding gap, increasing every year due to the growing needs of an ageing population, with the health burden shifting towards non-communicable diseases (NCDs), now the major cause of death in emerging markets. Traditional sources of healthcare funding struggle to increase budgets sufficiently to cover this gap and only about 4% of private health care investments focus on diseases that primarily affect low- and middle-income countries.
In middle-income countries, private investors often focus on extending established businesses, including developing private hospital capacity, targeting consumers already benefiting from quality healthcare. As a result, an insufficient amount of private capital is invested in strengthening healthcare systems for everyone.
Why is this the case? We discussed with senior health executives investing in Lower and Middle Income Countries (LMIC) and the following reasons emerged:
-Small market size. Scaling innovations in healthcare requires dealing with country-specific regulatory frameworks and competing interest groups, resulting in high market entry cost.
-Talent. Several LMICs are losing nurses and doctors but also business and finance professionals to European and North American markets due to the lack of local opportunities and a significant difference in salaries.
-Untested business models with relatively low gross margins. Providing healthcare requires innovative business models where consumers’ willingness to pay often needs to be demonstrated over a significant period of time. Additionally, relatively low gross margins drive the need for scale to leverage administrative costs, which increases risk.
-Government Relations. The main buyer of health-related products and services is government; yet the relationship between public and private sectors often lacks trust, creating barriers to successful collaboration. Add to that significant political risk, as contracts can be cancelled by incoming administrations after elections. Many countries also lack comprehensive technology strategies to successfully manage technological innovation.
-Complexity of donor funding. A significant portion of healthcare is funded by private donors, whose priorities might not always be congruent with the health priorities of the government.
Notwithstanding these barriers, healthcare, specifically in middle-income settings, could present an attractive value proposition for private investors:
-Economic growth rates. A growing middle class is expanding the potential market for healthcare products and services.
-Alignment of incentives. A high ratio of out-of-pocket payments for healthcare services is often associated with low quality. However, innovative business models can turn out of pocket payments into the basis for a customer-centric value proposition, as the provider is required to compete for a share of disposable income.
-Emergence of National Health Insurance Schemes. South Africa, Ghana, Nigeria and others are building national health insurance schemes, increasing a population’s ability to fund healthcare services and products.
-Increased prevalence of NCDs. Given the increasing incidence of chronic diseases and the potential of using technology to address these diseases, new business opportunities for private investment exist.
Based on the context above, several areas in healthcare delivery can present compelling opportunities for private companies.
-Aggregation of existing players.
-Leveraging primary care infrastructure. Retail companies can leverage their real estate, infrastructure and supply chains to deploy primary care services at greater scale than is currently the case.
-Telemedicine. Telecommunications providers can leverage their existing infrastructure and customer base to provide payment mechanisms and telehealth services at scale. As seen during the COVID-19 pandemic, investment in telemedicine can ensure that patients receive timely and continuous care in spite of restrictions and lockdowns.
-Cost effective diagnostics. Diagnostic tools operated by frontline workers and combined with the expertise of specialists can provide timely and efficient care.
To fully realize these opportunities, government must incentivise innovation, provide clear regulatory frameworks and, most importantly, ensure that health priorities are adequately addressed.
Venture capital and private equity firms as well as large international corporations can identify the most commercially viable solutions and scale them into new markets. The ubiquity of NCDs and the requirement to reduce costs globally provides innovators with the opportunity to scale their tested solutions from LMICs to higher income environments.
Successful investment exits in LMICs and other private sector success stories will attract more private capital. Governments that enable and support private investment in their healthcare systems would, with appropriate governance and guidance, generate benefits to their populations and economies. The economic value of healthy populations has been proven repeatedly, and in the face of COVID-19, private sector investment can promote innovation and the development of responsible, sustainable solutions.
Faith – the diabetic mother we introduced at the beginning of this article - could keep her client. As a stable patient, she could measure her glucose level at home and enter the results in an app on her phone, part of her monthly diabetes programme with the company that runs the health centre. She visits the nurse-led facility at the local taxi stand on her way to work when her app suggests it. The nurse in charge of the centre treats Faith efficiently, and, if necessary, communicates with a primary care physician or even a specialist through the telemedicine functionality of her electronic health system.
Improving LMIC health systems is not only a business opportunity, but a moral imperative for public and private leaders. With the appropriate technology and political will, this can become a reality.
6. How could COVID-19 change the way we pay for health services?
The emergence of the new severe acute respiratory syndrome coronavirus (SARS-Cov-2), causing the coronavirus disease 2019 (COVID-19), has challenged both developing and developed countries.
Countries have approached the management of infections differently. Many people are curious to understand their health system’s performance on COVID-19, both at the national level and compared to international peers. Alongside limited resources for health, many developing countries may have weak health systems that can make it challenging to respond adequately to the pandemic.
Even before COVID-19, high rates of out-of-pocket spending on health meant that every year, 800 million people faced catastrophic healthcare costs,100 million families were pushed into poverty, and millions more simply avoided care for critical conditions because they could not afford to pay for it.
The pandemic and its economic fallout have caused household incomes to decline at the same time as healthcare risks are rising. In some countries with insurance schemes, and especially for private health insurance, the following questions have arisen: How large is the co-payment for a COVID-19 test? If my doctor’s office is closed, will the telemedicine consultation be covered by my insurance? Will my coronavirus care be paid for regardless of how I contracted the virus? These and other doubts can prevent people from seeking medical care in some countries.
In Nigeria, like many other countries in Africa, the government bears the costs associated with testing and treating COVID-19 irrespective of the individual’s insurance status. In the public health sector, where COVID-19 cases are treated, health workers are paid monthly salaries while budgets are allocated to health facilities for other services. Hospitals continue to receive budget allocations to finance all health services including the management and treatment of COVID-19. That implies that funds allocated to address other health needs are reduced and that in turn could affect the availability and quality of health services.
Although health workers providing care for COVID-19 patients in isolation and treatment centres in Nigeria are paid salaries that are augmented with a special incentive package, the degree of impact on the quality improvement of services remains unclear. The traditional and historical allocation of budgets does not always address the needs of the whole population and could result in poor health services and under-provision of health services for COVID-19 patients.
In some countries, the reliance on out-of-pocket funding is hardly better for private providers, who encounter brand risks, operational difficulties, and – in extreme cases – the risk of creating “debtor prisons” as they seek to collect payment from patients. Ironically, despite the huge demand for medical services to diagnose and treat COVID-19, large healthcare institutions and individual healthcare practitioners alike are facing financial distress.
Dependence on a steady stream of fee-for-service payments for outpatient consultations and elective procedures is leading to pay cuts for doctors in India, forfeited Eid bonuses for nurses in Indonesia, and hospital bankruptcies in the United States. In a recent McKinsey & Company survey, 77% of physicians reported that their business would suffer in 2020, and 46% were concerned about their practice surviving the coronavirus pandemic.
COVID-19 is exposing how fee-for-service, historical budget allocation and out-of-pocket financing methods can hinder the performance of the health system. Some providers and health systems that deployed “value-based” models prior to the pandemic have reported that these approaches have improved financial resilience during COVID-19 and may support better results for patients. Nevertheless, these types of innovations do not represent the dominant payment model in any country.
How health service providers are paid has implications for whether service users can get needed health services in a timely fashion, and at an appropriate quality and an affordable cost. By shifting from fee-for-service reimbursements to fixed "capitation" and performance-based payments, these models incentivize providers to improve quality and coordination while also guaranteeing a baseline income level, even during times of disruption.
Health service providers could be paid either in the form of salaries, a fee for services they provide, by capitation (whether adjusted or straightforward), through global budgets, or by using a case-based payment system (for example, the diagnostics-related groups), among others. Because there are different incentives to consider when adopting any of the methods, they could be combined to achieve a specific goal. For example, in some countries, health workers are paid salaries, and some specific services are paid on a fee-for-service basis.
Ideally, health services could be purchased strategically, incorporating aspects of provider performance in transferring funds to providers and accounting for the health needs of the population they serve.
In this regard, strategic purchasing for health has been advocated and should be highlighted as crucial with the emergence of the COVID-19 pandemic. There is a need to ensure value in the way health providers are paid, inter alia to increase efficiency, ensure equity, and improve access to needed health services. Value-based payment methods, although not new in many countries, provide an avenue to encourage long-term value for money, better quality, and strategic purchasing for health, helping to build a healthier, more resilient world.
7. Lessons in integrated care from the COVID-19 pandemic
Since the start of the COVID-19 pandemic, people suffering non-communicable diseases (NCDs) have been at higher risk of becoming severely ill or dying. In Italy, 96.2% of people who died of COVID-19 lived with two or more chronic conditions.
Beyond the pandemic, cardiovascular disease, cancer, respiratory disease and diabetes are the leading burden of disease, with 41 million annual deaths. People with multimorbidity - a number of different conditions - often experience difficulties in accessing timely and coordinated healthcare, made worse when health systems are busy fighting against the pandemic.
Here is what happened in China with Lee, aged 62, who has been living with Chronic Obstructive Pulmonary Disease (COPD) for the past five years.
Before the pandemic, Lee’s care manager coordinated a multi-disciplinary team of physicians, nurses, pulmonary rehabilitation therapists, psychologists and social workers to put together a personalized care plan for her. Following the care plan, Lee stopped smoking and paid special attention to her diet, sleep and physical exercises, as well as sticking to her medication and follow-up visits. She participated in a weekly community-based physical activity program to meet other COPD patients, including short walks and exchange experiences. A mobile care team supported her with weekly cleaning and grocery shopping.
Together with her family, Lee had follow-up visits to ensure her care plan reflected her recovery and to modify the plan if needed. These integrated care services brought pieces of care together, centered around Lee’s needs, and provided a continuum of care that helped keep Lee in the community with a good quality of life for as long as possible.
Since the COVID-19 outbreak, such NCD services have been disrupted by lockdowns, the cancellation of elective care and the fear of visiting care service. These factors particularly affected people living with NCDs like Lee. As such, Lee was not able to follow her care plan anymore. The mobile care team was unable to visit her weekly as they were deployed to provide COVID-19 relief. Lee couldn’t participate in her community-based program, follow up on her daily activities, or see her family or psychologists. This negatively affected Lee’s COPD management and led to poor management of her physical activity and healthy diet.
The pandemic highlights the need for a flexible and reliable integrated care system to enable healthcare delivery to all people no matter where they live, uzilizing approaches such as telemedicine and effective triaging to overcome care disruptions.
Lee’s care manager created short videos to assist her family through each step of her care and called daily to check in on the implementation of the plan and answer questions. Lee received tele-consultations, and was invited to the weekly webcast series that supported COPD patient communities. When her uncle passed away because of pneumonia complications from COVID-19 in early April, Lee’s care manager arranged a palliative care provider to support the family through the difficult time of bereavement and provided food and supplies during quarantine. Lee could even continue with her physical activity program with an online training coach. There were a total of 38 exercise videos for strengthening and stretching arms, legs and trunk, which she could complete at different levels of difficulty and with different numbers of repetitions.
Lee’s case demonstrates that early detection, prevention, and management of NCDs play a crucial role in a global pandemic response. It shows how we need to shift away from health systems designed around single diseases towards health systems designed for the multidimensional needs of individuals. As part of the pandemic responses, addressing and managing risks related to NCDs and prevention of their complications are critical to improve outcomes for vulnerable people like Lee.
How to design and deliver successful integrated care
The challenge for the successful transformation of healthcare is to tailor care system-wide to population needs. A 2016 WHO Framework on integrated people-centered health services developed a set of five general strategies for countries to progress towards people-centered and sustainable health systems, calling for a fundamental transformation not only in the way health services are delivered, but also in the way they are financed and managed. These strategies call for countries to:
-Engage and empower people / communities: an integrated care system must mobilize everyone to work together using all available resources, especially when continuity of essential health and community services for NCDs are at risk of being undermined.
-Strengthen governance and accountability, so that integration emphasizes rather than weakens leadership in every part of the system, and ensure that NCDs are included in national COVID-19 plans and future essential health services.
-Reorient the model of care to put the needs and perspectives of each person / family at the center of care planning and outcome measurement, rather than institutions.
-Coordinate services within and across sectors, for example, integrate inter-disciplinary medical care with social care, addressing wider socio-economic, environmental and behavioral determinants of health.
-Create an enabling environment, with clear objectives, supportive financing, regulations and insurance coverage for integrated care, including the development and use of systemic digital health care solutions.
Whether due to an unexpected pandemic or a gradual increase in the burden of NCDs, each person could face many health threats across the life-course.
Only systems that dynamically assess each person’s complex health needs and address them through a timely, well-coordinated and tailored mix of health and social care services will be able to deliver desired health outcomes over the longer term, ensuring an uninterrupted good quality of life for Lee and many others like her.
8. Why access to healthcare alone will not save lives
Joyce lies next to 10 other women in bare single beds in the post-partum recovery room at a rural hospital in Uganda. Just an hour ago, Joyce gave birth to a healthy baby boy. She is now struggling with abdominal pain. A nurse walks by, and Joyce tries to call out, but the nurse was too busy to attend to her; she was the only nurse looking after 20 patients.
Another hour passes, and Joyce is shaking and sweating profusely. Joyce’s husband runs into the corridor to find a nurse to come and evaluate her. The nurse notices Joyce’s critical condition - a high fever and a low blood pressure - and she quickly calls the doctor. The medical team rushes Joyce to the intensive care unit. Joyce has a very severe blood stream infection. It takes another hour before antibiotics are started - too late. Joyce dies, leaving behind a newborn son and a husband. Joyce, like many before her, falls victim to a pervasive global threat: poor quality of care.
Adopted by United Nations (UN) in 2015, the Sustainable Development Goals (SDG) are a universal call to action to end poverty, protect the planet and ensure that all enjoy peace and prosperity by 2030. SDG 3 aims to ensure healthy lives and promote wellbeing for all. The 2019 UN General Assembly High Level Meeting on Universal Health Coverage (UHC) reaffirmed the need for the highest level of political commitment to health care for all.
However, progress towards UHC, often measured in terms of access, not outcomes, does not guarantee better health, as we can see from Joyce’s tragedy. This is also evident with the COVID-19 response. The rapidly evolving nature of the COVID-19 pandemic has highlighted long-term structural inefficiencies and inequities in health systems and societies trying to mitigate the contagion and loss of life.
Systems are straining under significant pressure to ensure standards of care for both COVID-19 patients and other patients that run the risk of not receiving timely and appropriate care. Although poor quality of care has been a long-standing issue, it is imperative now more than ever that systems implement high-quality services as part of their efforts toward UHC.
Poor quality healthcare remains a challenge for countries at all levels of economic development: 10% of hospitalized patients acquire an infection during their hospitalization in low-and-middle income countries (LMIC), whereas 7% do in high-income countries. Poor quality healthcare disproportionally affects the poor and those in LMICs. Of the approximately 8.6 million deaths per year in 137 LMICs, 3.6 million are people who did not access the health system, whereas 5 million are people who sought and had access to services but received poor-quality care.
Joyce’s story is all too familiar; poor quality of care results in deaths from treatable diseases and conditions. Although the causes of death are often multifactorial, deaths and increased morbidity from treatable conditions are often a reflection of defects in the quality of care.
The large number of deaths and avoidable complications are also accompanied by substantial economic costs. In 2015 alone, 130 LMICs faced US $6 trillion in economic losses. Although there is concern that implementing quality measures may be a costly endeavor, it is clear that the economic toll associated with a lack of quality of care is far more troublesome and further stunts the socio-economic development of LMICs, made apparent with the COVID-19 pandemic.
Poor-quality care not only leads to adverse outcomes in terms of high morbidity and mortality, but it also impacts patient experience and patient confidence in health systems. Less than one-quarter of people in LMICs and approximately half of people in high-income countries believe that their health systems work well.
A lack of application and availability of evidenced-based guidelines is one key driver of poor-quality care. The rapidly changing landscape of medical knowledge and guidelines requires healthcare workers to have immediate access to current clinical resources. Despite our "information age", health providers are not accessing clinical guidelines or do not have access to the latest practical, lifesaving information.
Getting information to health workers in the places where it is most needed is a delivery challenge. Indeed, adherence to clinical practice guidelines in eight LMICs was below 50%, and in OECD countries, despite being a part of national guidelines, 19-53% of women aged 50-69 years did not receive mammography screening.4 The evidence in LMICs and HICs suggest that application of evidence-based guidelines lead to reduction in mortality and improved health outcomes.
Equally, the failure to change and continually improve the processes in health systems that support the workforce takes a high toll on quality of care. During the initial wave of the COVID-19 pandemic, countries such as Taiwan, Hong Kong, Singapore and Vietnam, which adapted and improved their health systems after the SARS and H1N1 outbreaks, were able to rapidly mobilize a large-scale quarantine and contact tracing strategy, supported with effective and coordinated mass communication.
These countries not only mitigated the economic and mortality damage, but also prevented their health systems and workforce from enduring extreme burden and inability to maintain critical medical supplies. In all nations, investing in healthcare organizations to enable them to become true “learning health care systems,” aiming at continual quality improvement, would yield major population health and health system gains.
The COVID-19 pandemic underscores the importance for health systems to be learning systems. Once the dust settles, we need to focus, collectively, on learning from this experience and adapting our health systems to be more resilient for the next one. This implies a need for commitment to and investment in global health cooperation, improvement in health care leadership, and change management.
With strong political and financial commitment to UHC, and its demonstrable effect in addressing crises such as COVID-19, for the first time, the world has a viable chance of UHC becoming a reality. However, without an equally strong political, managerial, and financial commitment to continually improving, high-quality health services, UHC will remain an empty promise.
*first published in: www.weforum.org




 By: N. Peter Kramer
By: N. Peter Kramer