by Robin Pomeroy*
-Senior advisor to the Director-General of the World Health Organization (WHO) Bruce Aylward talks testing and how to break the COVID-19 transmission chain.
-Lockdowns will likely last more than two weeks.
-To hold off a second wave, governments must rapidly find and test suspect cases, isolate and treat confirmed cases, and quarantine others.
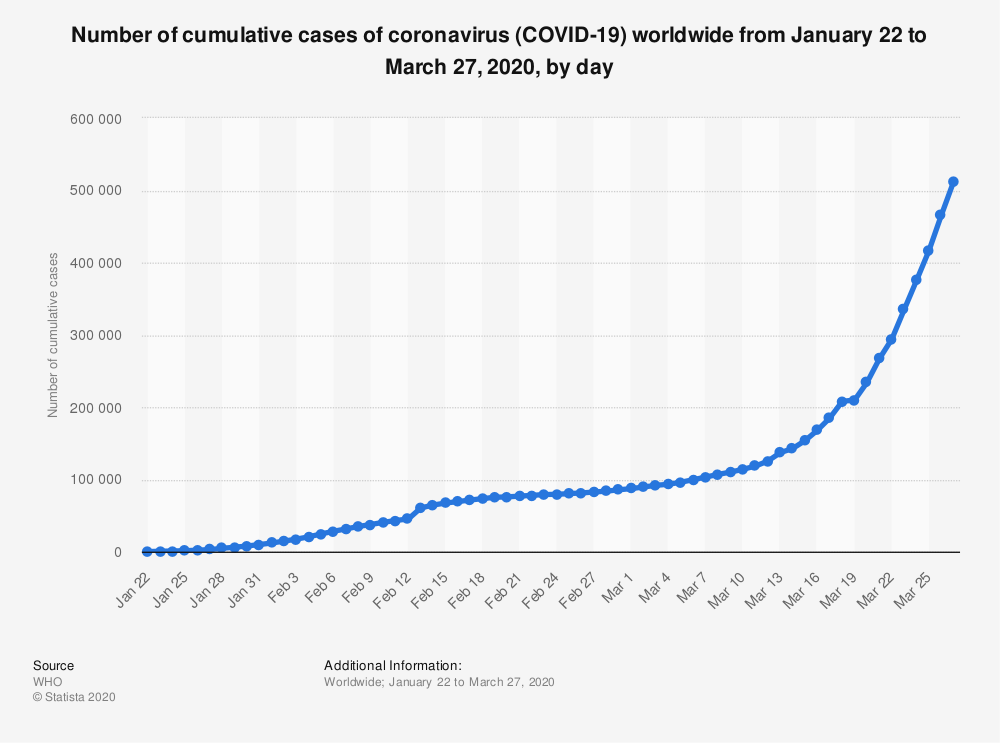
The COVID-19 pandemic is surging around the world and China is preparing itself for a second wave of infections. World Health Organization Director-General Tedros Adhanom Ghebreyesus told G20 leaders this week, "The pandemic is accelerating at an exponential rate."
Bruce Aylward, senior advisor to the WHO Director-General, says governments must keep their populations under lockdown while chasing down every suspect case for testing, and treating and isolating those who test positive.
Below is an edited transcript of my conversation with Bruce Aylward, which you can listen to in full here. Subscribe to our World vs Virus podcast here.
Many of the people listening to this are in some form of lockdown and will want to know how long will it last.
Well, probably the best indicator of how long this might last comes from China, because it’s the only country that has truly taken a rapidly escalating COVID-19 outbreak and really turned the corner and brought it down.
And if you look across China, across the 31 provinces, all of which were affected at one point or another, the longest and most difficult, of course, was Wuhan, which remains locked down. It will be nearly 10 weeks by the time they will have lifted there – all of February, March, and much of April. Now, there are many other provinces, however, that were able to manage this with a much shorter shutdown period, that ranged anywhere from a month to two months. It really depends on the context how well control measures bite or take the heat out of this outbreak. But it will be more than a couple of weeks anywhere, almost definitely.
That doesn’t sound too long. I guess the risk we’re all worried about is a second wave. People keep quoting the Spanish flu pandemic from a century ago.
There’s really two scenarios you could think of. What countries have done with all these slowdowns and shutdowns in workplaces and educational institutions and in society is they really slowed down the rate of increase of the COVID outbreaks. But they actually haven’t broken the transmission chain. That really requires finding every single case, testing every suspect case, confirming them, isolating the suspect cases, quarantining the others. And you really have to do those transmission chain-level measures as well as the big shutdowns and slowdowns and lockdowns if you want this thing really to turn around.
So, when I give an optimistic timeline, it’s if you were doing all of that. Now, most countries are scrambling just to get the big measures in place just to treat the most severe patients. And that’s what worries me a little bit in the West, that it might take a little bit longer to take the heat out of this thing. But I always want to be careful because we’re dealing with a biologic process that’s happening in the context of changes in seasons and other factors that just make some of this, frankly, unpredictable. The key thing right now is doing as much as you can to save lives, it means training people. But it also means trying to slow down that outbreak at the same time.
On the testing issue, there seem to be different interpretations around the world of what should be happening. What is the World Health Organization’s recommendation for testing? Is it test everyone you can? What is the recommendation?
Well, that’s a really good question because there’s a lot of interpretation even of our recommendation. So, let’s try and set that record straight. What you do in a situation like this is always test the suspect cases. You don’t want to test everybody because, number one, it will waste a lot of resources because a lot of people won’t be infected. The other thing is it gives a lot of people a false sense of security. They’ll think, ‘Oh, the test was negative. So, I’m safe.’ And you have to take any tests like that in the context of the risk.
If you test a whole bunch of people who aren’t safe the test will tell you, usually, that they’re not safe, but then you can have false positives, false negatives, all sorts of problems. So, what you really want – for the reasons of issues around the test itself, but also issues around the amount of resource available – is to test the suspect cases.
What our recommendation is: test, test, test. But test the suspect cases because it’s like that old story – my family’s getting sick of hearing this one – but, you know, they once asked that famous bank robber, Willie, ‘Why do you rob banks?’ And he says, ‘Well, that’s where the money is.’ And so, why do you test suspect cases? Because that’s where most of the COVID virus is. So, you find those and if we test everyone else, we’ll have a lot of other problems, frankly.
And if we don’t test in the way you’re suggesting, that will increase the risk of a second wave?
Well, what’s going to happen is that people are getting advice that says if you feel unwell or you think you might have caught it, stay home until you feel better. Now, the reality is they may well have COVID. If they stay home, first of all, and they’re not sure they have COVID, they won’t take the incredible precautions necessary not to infect the rest of their family if they live with people. But the bigger problem is that within two or three or four or five days, they’re going to feel a lot better and they’re going to say to themselves, ‘Gosh, I heard COVID was a terrible disease. So, I must have just had a cold or something.’ And I’ll wander back out there into society and supermarkets and other forums. And what’s going to happen, though, is they can still infect people because even though you feel better, you can still be infectious for up to 14 days and possibly even longer after you’ve recovered from the disease. So, for that reason, we really want people to know their status because it just helps them be better citizens and take better care of themselves and their families.
We saw that Spain’s death rate, following Italy’s, overtook that of China’s. Is there any way of saying why those two countries are getting it so heavily? Or is it just the way of these things and many other countries will be going down that route in a week’s time or so?
Well, there’s a combination of factors. When we look at a country like Italy or Spain and we think, ‘Well, why did they get so badly hit?’ Part of it is just temporal. But by that, I mean timing. They got hit earlier than some of the others. And then some of the high death rates that we’re seeing, etc. can be associated with multiple factors. We hear about this in the news all the time. Italy is the second oldest population in the world after Japan, of course. It can also be the fact that we’re mainly seeing the severe cases that are hitting the hospitals and not all the mild cases are getting tested. So, we have a falsely high death rate and there’s other factors that can be at play as well.
What I always remind people is all of that is happening against a background of biologic processes in large populations that we don’t fully understand. We’ve known this disease for 12 weeks. Even diseases that we’ve known for decades, we still don’t know everything about why they express themselves in different ways and different populations. But what we have learned is this virus has the propensity to cause severe disease, societal disruption, massive outbreaks, economic disruption in any environment. We’ve seen it now in the Middle East. We’ve seen it in Asia. We’ve seen it in Europe. And what it tells us everywhere is: be prepared, be ready, take every step you possibly can to try and prevent the explosive outbreaks we’re seeing in places like Spain and Italy.
You’ve worked on outbreaks of infectious diseases around the world, including Ebola. What’s different about COVID-19 from all of these others that we got to know?
Over the last 20-30 years now, I’ve worked with large-scale infectious disease outbreaks, as have many, many of my colleagues to be clear. We’ve worked in Ebola outbreaks. We’ve worked in polio outbreaks, measles outbreaks, yellow fever outbreaks, the huge Zika outbreak that we saw just two years ago. And when we look at this COVID outbreak, what myself and my colleagues often discuss is it brings many of those pieces together. Zika, for example, was almost a pandemic. It spread. That virus can be found almost all around the world, but it affected one population and it hit one area of the world much more, much worse than other areas.
We’ve seen pandemic flu as well, but with a much lower mortality rate. We’ve seen high mortality diseases like Ebola, for example, but in very discrete areas. What’s different about this one is it brings out the wide geographic spread of a pandemic together with the high mortality rates. And together with it being a respiratory pathogen, which means it spreads out much more rapidly. So, this really brings together so many of those things that made each one of the other ones I mentioned dangerous individually and often for discrete areas and certain sub-populations. This disease affects the global population, basically all age groups. Some are hit worse. This is a dangerous combination of many of the worst attributes we’ve seen of other viruses.
At danger of oversimplifying that, is it that COVID-19 is just far more infectious? It’s easier to transmit?
Well, there are other diseases that are even more infectious or spreading more rapidly. For example, people always quote this reproductive number and say, ‘Wow, COVID has a reproductive number of 2.5.’ Measles has a reproductive number that’s over 10. It can be spread much more efficiently. Flu can spread much more quickly. It has a much shorter serial interval than this one. So, again, it’s the combination which makes this virus so difficult.
Looking ahead now, does the World Health Organization have certain milestones you’re looking ahead to? What are the things you’re fearing might happen? And what are the positive milestones?
Well, first of all, you don’t wait (for positive milestones). You push for those things. You push very hard. And what we really are looking at is how many places in the world can find their suspect cases and test them within 48 hours of their onset of symptoms. Because when you get that number very, very high, you’re going to understand the magnitude of what you’re dealing with. How many countries can effectively isolate their cases within 24 hours? Because when you can do that, you know that you’re getting the known virus out of the community. It’s not infecting other people and you’re getting in front of it. And then similarly, we look at quarantine rates, etc. So, there’s a whole bunch of indicators that tell us whether a country is on top of the measures needed to slow it down.
The other things we look at, of course, is how well are the lifesaving measures working? And there, you’re looking at the case fatality rates in different age groups and different sub-groups. But what’s most important is looking at what’s happening to that epidemic trend. Is the rate of new cases slowing and has it actually turned that outbreak? But that can be due to a number of factors. So, some people are just watching those curves go up and seeing them turn. But what you want to see is the combination of the curve plus the response measures. And that’s why when I was in China and doing a briefing at the end of it, I would never show just a curve. I would also say, ‘Here’s the curve and here’s all the things that were being done to change that curve.’ And that’s what we need to see: what does the curve look like? What are the big measures in place? Are they at the performance levels we want?’ Because that will tell you in maybe two or three weeks if that curve is going to bend.
And, when the curves have bent, you want to be sure that it’s for the right reasons and not just because testing dropped off or surveillance. So, it’s a combination: what’s happening to the curve and the response measures on top of it. Any one of the two only gives you a partial understanding.
So those are the things we’ll be looking out for in the coming weeks.
Part of it will be watching – we’ll be watching the curves but the response measures we’ll be pushing. That’s the part we control. This is what’s so important about COVID: we went into China wondering about this disease. There was a lot we didn’t know. We knew it was a respiratory pathogen. We knew we didn’t have a vaccine. And that usually means you’re trying to do as much as possible just to save lives because the virus is always going to be in front of you. And what we learned was, to our surprise, old-fashioned case-finding, isolation, quarantine can actually slow down a respiratory disease. So, I’ll come back to that again and again and again because countries are now taking extraordinary measures to put shutdowns and slowdowns and lockdowns in place. But unless you’re doing the other part, when they lift the big measures, this thing could take off again. And we want to make sure that when you lift the measures, the virus stays down.
I’d like to throw out some rapid-fire questions. So, if I get COVID-19 and I recover: am I then immune from getting it again?
Probably. We don’t know 100%, but most of what we know about coronaviruses tells us that you will develop immunity against this one. We still haven’t got the tests to prove it. So, it’s going to take a little time, but the expectation is yes.
How long does it linger on surfaces? We’re buying things, bringing things into our houses. How much do we need to worry about the virus being on things?
In most cases, it’s going to be a very short period. Remember, viruses can only survive in human cells or the living cells of an animal or human. As soon as it’s out a virus is dying, it’s not replicating anymore. So, the amount of virus is dropping very, very fast. Within a couple of hours, it’s gone to low levels. In your day-to-day life, that’s not a problem. However, if you have a case living with you or a contact, those people are spewing out a lot of virus on a regular basis. So, that’s a different setting altogether if they’re infected. And in that situation, you have to take extraordinary measures to make sure the living surfaces, etc. are all clean. That’s a different matter. Like in hospitals with sick, sick patients.
It can be carried in the air. Am I safe to go out? To walk around, respecting distances, or go for a run in Geneva?
You’re absolutely safe as long as you maintain the right distances. Because remember: this is a virus that is a respiratory pathogen or a virus, but it moves in little droplets. And these droplets, they fall very quickly. They don’t float in the air. So, what happens is if I cough, these would travel about a metre or maybe a little bit further. And for that reason, we say it should be a metre, two metres between two people. Or for your imperial audiences, three feet, six feet away, the length of a llama – someone told me that yesterday. But the important thing is if you have that distance, you’re safe.
Now, there are some situations where it will happen in hospitals where the virus can get what they call aerosolized. And that’s what people worry about, where it might be in little tiny particles that hang in the air longer. But that’s an extraordinary situation. It’s not what you have to worry about on a day-to-day basis. The key here is to make it difficult for the virus to get between you and other people. That’s how I explain it to people. It’s just a virus. It’s got to get from one person to another. Make it hard for the virus. We can beat this.
*Digital Editor, World Economic Forum
**first published in: www.weforum.org




 By: N. Peter Kramer
By: N. Peter Kramer

